The exploration of mindfulness-based interventions (MBIs) presents an exciting opportunity within health and psychological research. This synopsis highlights evidence-based applications and potential challenges of mindfulness programs, apps, and long-term practices in addressing stress, anxiety, and burnout, focusing on studies published between 2019 and 2024.
This work is part of a comprehensive systematic review, which examined over 4,000 academic articles from 2009 to 2024, resulting in over 200 citations. For those interested in a deeper dive into the research landscape, a detailed annotated bibliography list is available for download.
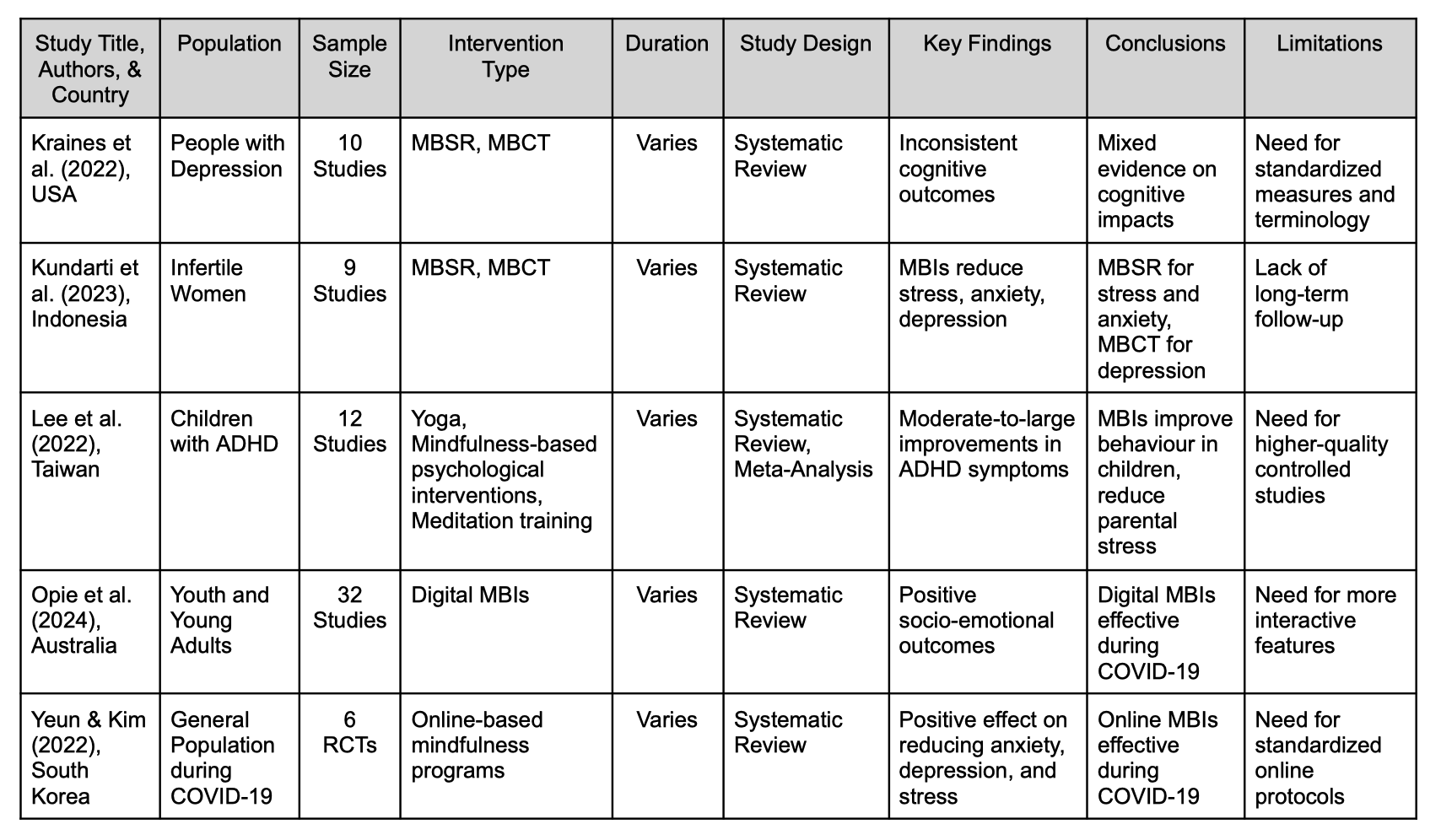
Summary of Key Findings
A medical student feels a familiar tightening in their chest as the morning sun casts a pink haze over their computer screen. The same rays warm the face of a chronically ill patient as they breathe through another procedure and dry the tears of a nurse sitting silently in her driveway. In a time when the unprecedented has become utterly precedent, anxiety, fear, and stress have compressed themselves into a thread that now connects us all. It is no surprise, then, that there has been a growing interest in exploring mindfulness-based interventions (MBIs) as a means to build emotional resilience against stress and anxiety, and to provide an accessible pathway for healing from burnout.
Mindfulness practices have been part of the Western world for decades, but research in this once-niche area has recently surged, particularly since the onset of the COVID-19 pandemic. While interest in MBIs has gained traction in several areas, there is a clear parallel between the start of the pandemic and an emerging focus on stress, anxiety, and burnout, particularly within the medical field. An analysis of 14 systematic reviews highlights several significant trends in this research area. Over the past five years, healthcare workers have been immersed in extreme stress, working gruelling hours while their bodies ache for much-needed rest, all while the emotional toll of worrying about their families and processing an overwhelming amount of death weighs heavily on their minds. In response to what felt like an insurmountable crisis, researchers acted with both creativity and urgency, rapidly developing initiatives such as team-based mindfulness programs aimed at improving communication, support, and cohesion within medical teams. Additional efforts focused on adapting existing MBIs, such as Mindfulness-Based Stress Reduction (MBSR), to help healthcare workers relieve stress, build resilience, and recover from burnout without adding further burden, and introducing digital MBIs as a cost-effective and scalable solution, particularly for healthcare workers in rural and underserved areas.
During this period, mindfulness research has also strongly influenced patient care, with a significant emphasis on enhancing emotional stability, managing pain, and fostering peer support among individuals with chronic illness. Similar to efforts made for healthcare workers, researchers have focused on adapting MBI programming to meet the needs of diverse patient groups. This includes modifying the frequency and duration of mindfulness sessions, incorporating movement-based practices for those who benefit from them, and tailoring specific aspects of MBIs to more effectively address the emotional and psychological needs of distinct populations. Interestingly, since 2015, there has also been growing interest in applying MBIs to family caregivers. The acknowledgment that family members often assume the role of full-time healthcare support for loved ones has led researchers to explore not only the impact of MBIs on stress, anxiety, and depression in caregivers but also the complexity of the relationship between individuals with chronic illness and their loved ones. Researchers suggest that caregivers who build emotional resilience and maintain their mental health may positively influence overall outcomes for those they support. This approach highlights the complexities of holistic patient care plans and underscores the need for nuanced, individualized care to encourage the best patient outcomes.
Finally, as researchers have worked diligently to sustain frontline workers and fortify the long-term resilience of patients managing chronic conditions at home, they have also diverted significant attention toward the future of healthcare—nursing and medical students. For over a decade, researchers have observed an alarming increase in mental health issues within this population, a trend that has only intensified since the onset of the COVID-19 pandemic. MBIs have become a focal point of research in this area, aiming to equip healthcare students with the skills necessary to manage stress, reduce anxiety, and ultimately prevent burnout as they transition into their professional roles. These efforts include adaptations of programs initially designed for active healthcare workers and patients, such as shorter and more flexible sessions tailored to students’ specific needs and concerns. Additionally, there is a strong interest in digital applications for MBIs, which offer a cost-effective, scalable, and fluid approach to mindfulness adapted to a generation of native technology users. As research in this sphere continues to develop, the hope is that by equipping the next generation of healthcare professionals with an armoury of tools to effectively relieve stress and regulate their emotions in healthy ways, not only will these students experience a reduction in academic-related stress and anxiety, but they will also have a robust set of tools to help mitigate the impact of burnout before it can truly take root in their lives.
While a future where mindfulness could cure the sick and heal our overburdened healthcare system would bring unimaginable relief to society at large, this area of research still faces significant challenges, limitations, and truths that must be addressed. For instance, although there has been significant progress in developing MBI applications for managing stress and anxiety, evidence consistently shows that mindfulness is not effective in addressing burnout. Researchers suggest that this is largely because burnout is deeply rooted in systemic issues that cannot be adequately addressed at the individual level. Additionally, current research in this area is hindered by methodological challenges common to the field, including small sample sizes, a lack of standardization in definitions, measurements, and study designs, as well as significant heterogeneity between studies, all of which complicate meta-analysis and data synthesis.
Looking ahead, researchers have made several recommendations to advance our understanding of mindfulness applications within the healthcare field. First and foremost, there is an urgent need for studies exploring the long-term efficacy of MBIs, particularly in the area of building and maintaining emotional resilience over time. These studies should investigate both the enduring impact of standardized programs like MBSR, as well as programs of varying frequency and duration, to ensure that we are maximizing the benefits of mindfulness practice while being mindful of the physical, emotional, and psychological constraints of those who provide and access medical services. Additionally, while it is increasingly recognized that burnout cannot be fully addressed on an individual level, both medical students and professionals may greatly benefit from the integration of mindfulness programs as part of a broader health-focused systemic change within the workplace, where policies, procedures, and culture are designed to support the regular practice of mindfulness. Moreover, the role of family caregivers is emerging as a critical area of research with the potential to significantly impact both patient outcomes and the broader healthcare system. Studies suggest that when caregivers are emotionally resilient and well-regulated, they not only contribute to better health outcomes for the patients they support but also help reduce the frequency of healthcare visits. This reduction in healthcare utilization indirectly eases the strain on an overburdened medical system. As such, incorporating MBIs tailored to the unique needs of family caregivers could be transformative, offering a dual benefit by improving the well-being of both caregivers and patients, while also contributing to the overall efficiency and sustainability of healthcare delivery. Finally, the area of digital MBIs holds considerable promise and warrants further exploration, as its broader applications could be transformative for the field. Specifically, current researchers recommend efforts be made to identify which populations would benefit most from this scalable solution, and how digital MBI applications can be tailored to address the unique cultural, socioeconomic, and demographic needs of diverse users, thereby optimizing outcomes.
Knowledge Synthesis
1. Chiodelli, R., Mello, L.T.N., Jesus, S.N., Beneton, E.R., Russel, T. & Andretta, I. (2022). Mindfulness-based interventions in undergraduate students: A systematic review. In Journal of American College Health: J of ACH (Vol. 70, Issue 3, pp. 791–800). https://doi.org/10.1080/07448481.2020.1767109
Chiodelli et al. (2022) state that the Institute for Public Policy in the UK reported a five-time increase in mental health issues reported to the university over the last ten years (2012 – 2022). Depression and anxiety are the most commonly reported mental health concerns, with the number of students reporting depression doubling and the number of suicidal students tripling over the last decade. This study aimed to review how MBIs are implemented within university settings. A total of 19 papers were included in the review, confirming a rise in mental health concerns among university-aged students, particularly in the rating of distress (83% of students reported being moderately to severely stressed).
The authors confirmed their hypothesis that MBIs effected a significant change in psychological distress. While they acknowledge that the standardized 8-week MBSR program has the most empirical research, the authors found that abbreviated MBI sessions may make MBI programming more accessible to students. This suggestion is aligned with previous recommendations for populations like nurses who are coping with high-demand situations. The idea of adapting the delivery of MBIs to meet populations where they are may increase the accessibility of MBIs for populations who cannot commit mentally or physically to the demands of a standard MBSR program as their primary intervention. This concept mirrors the concepts used in dialectical behaviour therapy (DBT), which focuses on accepting where we are while building skills to change our situation over time.
2. Christodoulou, L., Parpottas, P., & Petkari, E. (2024). Psychological interventions to enhance positive outcomes in adult cancer caregivers: A systematic review. Journal of Health Psychology, 29(7), 747-769. https://doi.org/10.1177/135910532412362
Christodoulou et al. (2024) evaluate the impact of mindfulness-based interventions (MBIs) on family caregivers (FCs) of cancer patients. This review aligns with previous reviews indicating that MBIs may enhance positive outcomes for FCs in mental health and general well-being. Similar to other reviews focusing on FCs, a call is made for future research to include follow-up evaluations to determine the longevity of MBIs on wellbeing outcomes.
The authors highlight an important sub-population within the chronic illness community in those who care for or who are emotionally, psychologically, and physically impacted by the illness of a loved one. While aspects of cancer treatment and survival have been widely studied in the wellness space, shining a spotlight on the psychological and physical burnout associated with constant caregiving is an important avenue for future research, as the health of caregivers is directly related to the overall health outcomes of the people they care for. Additionally, understanding that the needs of caregivers may extend beyond the end of patient treatment (especially in terms of palliative care) may warrant the inclusion of FC’s health needs within patient treatment plans to maintain the health of the overall family unit.
3. Kajee, N., Montero-Marin, J., Saunders, K. E., Myall, K., Harriss, E., & Kuyken, W. (2024). Mindfulness training in healthcare professions: a scoping review of systematic reviews. Medical Education, 58(6), 671-686. https://doi.org/10.1111/medu.15293
Kajee et al. (2024) perform a scoping review of systematic reviews evaluating the effectiveness of Mindfulness-Based Interventions (MBIs) on the mental health, well-being, and communication skills of healthcare professionals (HCPs). The authors review 16 studies and conclude that MBIs generally improve mental health and well-being across different HCP groups, though results for burnout are inconclusive. The authors also note that HCPs outside of medicine and nursing are underrepresented in the literature. Despite the promising outcomes for mental health and empathy, the authors emphasize the need for more research addressing the high level of stress and burnout attributed to the demanding working conditions in this population.
This review highlights a significant limitation for studies focused on HCPs, suggesting that while MBIs may benefit this population, there are more comprehensive solutions for severe occupational stress and burnout. The authors rightly call for improved working conditions rather than solely relying on individual resilience-building interventions like MBIs, which resonates with our critique of the current neoliberal approach to healthcare. The authors also discuss the current state of MBI research, broadly criticizing the lack of standardized measures and operational definitions, lack of transparency in data reporting, and continuous bias, mirroring calls for more rigorous research methods and higher reporting standards found in previous studies reviewed for this project.
4. Xunlin, N. G., Lau, Y., & Klainin-Yobas, P. (2020). The effectiveness of mindfulness-based interventions among cancer patients and survivors: a systematic review and meta-analysis. Supportive Care in Cancer, 28, 1563-1578. https://doi.org/10.1007/s00520-019-05219-9
Xunlin et al. (2019) conduct a systematic review and meta-analysis assessing the effectiveness of mindfulness-based interventions (MBIs) in improving anxiety, depression, fatigue, and stress in people with cancer and cancer survivors. The authors reviewed 29 randomized controlled trials (RTCs) and found that MBIs significantly improved all symptoms of interest. Among the MBIs evaluated, mindfulness-based art therapy (MBAT) shows the strongest effects on reducing anxiety and depression, followed by mindfulness-based stress reduction (MBSR) and mindfulness-based care recovery (MBCR). The review concludes that MBIs might be effective as an adjunct therapy for managing cancer-related symptoms across different types of cancer.
This review highlights the significant benefits of MBIs in improving psychological and physical well-being among cancer patients and survivors. The notable effects observed across participants underscore the importance of integrating MBIs into standard cancer care plans. The particularly strong impact of mindfulness-based art therapy suggests that creative expression through art may offer additional therapeutic benefits for those struggling with cancer-related distress. However, variability across MBIs echoes previous studies calling for individualized approaches tailored to each person’s unique needs.
5. Yeun, Y. R., & Kim, S. D. (2022). Psychological effects of online-based mindfulness programs during the COVID-19 pandemic: A systematic review of randomized controlled trials. International journal of environmental research and public health, 19(3), 1624. https://pubmed.ncbi.nlm.nih.gov/35162646/
Yeun and Kim (2022) investigate the psychological impact of online-based mindfulness programs during the COVID-19 pandemic. The authors reviewed six randomized controlled trials (RCTs) and found that online-based mindfulness interventions may have a positive effect on reducing anxiety, depression, and stress in both clinical and general populations during the quarantine period. However, despite these positive findings, the authors reiterate the need for standardized online protocols and more rigorous research methodologies to provide consistent and reliable results in this area.
Interestingly, this is one of the first studies reviewed to recommend mindfulness-based interventions (MBIs) as a complementary or supplemental intervention to traditional Western treatments for stress, anxiety, and depression. Echoing other recent studies, the authors emphasize the importance of utilizing available technology to create personalized care for groups with diverse needs. They also stress the need for continued research across different populations and cultural contexts to understand the efficacy and applicability of these interventions fully.